Diabetes is affecting an increasing number of people – especially younger people. At the same time, more and more studies and field reports are now confirming that the widespread disease type 2 diabetes is curable. It’s not only nutrition that’s crucial here, but lifestyle as a whole.
What is Diabetes?
Diabetes mellitus is a chronic metabolic disease that leads to elevated blood sugar levels and has serious health consequences.
Elevated Blood Sugar Level
In the morning, after about eight hours of fasting, what’s referred to as the “fasting blood sugar level” in healthy people is about 65 – 100 mg/dl. If this value is more than 125 mg/dl, then it’s a strong indication of diabetes, as well as values of over 200 mg/dl measured in a non-fasting state. Also, if the long-term blood sugar level, HbA1c, is 6.5% (48 mmol/mol) or higher, that means diabetes is present in the body.
Types 1 and 2 Diabetes
There are two types of diabetes: type 1 and type 2, with type 2 affecting about 90% of people with diabetes overall. According to estimates, the total number of people with this disease worldwide is about 347 million. A study by the Robert Koch Institute shows that 7.2% of adults in Germany are already affected – and this trend is rising (1).
Type 1 Diabetes: Autoimmune Disease
Type 1 diabetes is an autoimmune disease.
Due to a faulty reaction of the immune system, antibodies attack the beta cells of the pancreas that are responsible for insulin production. This gradually destroys them until they can no longer produce insulin at all.
Insulin is the hormone that docks at the cell receptors and transports the sugar or glucose out of the blood and into the cells. Here’s the consequence of a lack of insulin: without this “door opener” for the sugar, this creates a lack of energy in the cells, and the sugar concentration in the blood ends up too high, which is also known as hyperglycemia.
Type 1 diabetes usually begins in childhood and adolescence. People with a genetic predisposition are particularly at risk here. Why the immune system identifies the cells of the pancreas as a danger and attacks them has not yet been conclusively clarified. But scientists suspect that, in addition to the genetic disposition, other factors can contribute to the immune system’s faulty reaction.
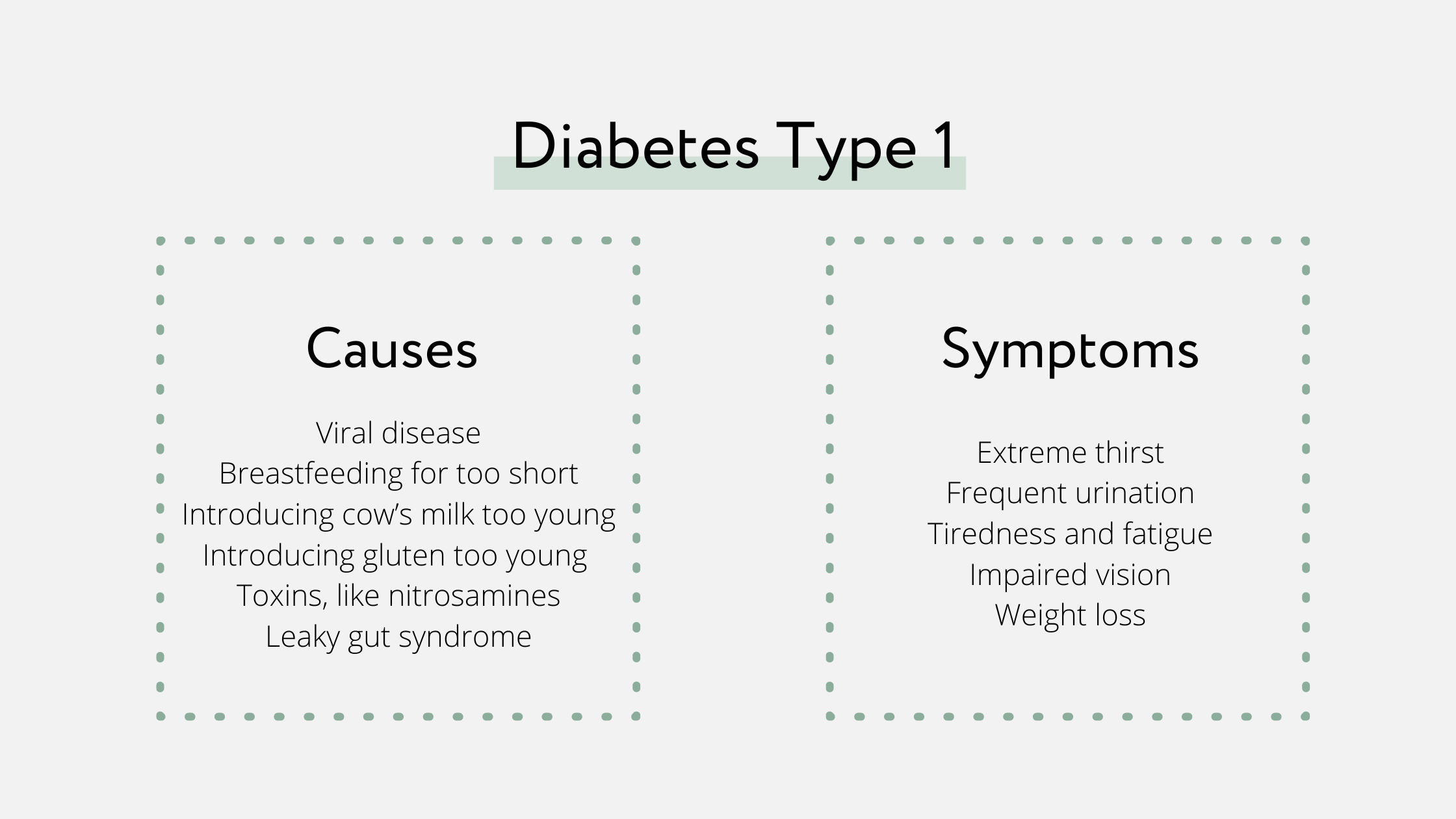
Possible Causes of Type 1 Diabetes:
- Viral disease, like mumps, which can cause the immune system to malfunction (2)
- Breastfeeding for too short of a period after giving birth (3)
- Introducing cow’s milk into childrens’ diets too young (4)
- Introducing gluten into children’s diets too young (5)
- Toxins, like nitrosamines (6)
- Autoimmune reaction due to leaky gut syndrome (7)
Symptoms Associated with Type 1 Diabetes:
Signs that may indicate the disease are:
- Extreme thirst
- Frequent urination
- Tiredness and fatigue
- Impaired vision
- Weight loss
Treatment: Insulin Injection
In order to maintain a normal metabolism, people with type 1 diabetes need injected insulin. Special training courses are available to teach people how to correctly dose insulin, get a feel for their own blood sugar levels, and make sure that the body is given enough insulin. The treatment includes permanently measuring one’s own blood sugar, calculating the carbohydrates in any food consumed, and injecting insulin accordingly.
In type 1 diabetes, the insulin-producing cells are destroyed by an autoimmune reaction of the body. So far, there is no way to regenerate and preserve these cells, so the most common treatment is to provide the body with insulin from the outside.

Type 2 Diabetes: Not a Sign of Old Age
Type 2 diabetes used to be called “adult-onset diabetes.” This term suggested that the disease was a symptom of old age. But this is wrong:
The reason we see type 2 diabetes in such a widespread capacity is clearly because of modern, Western lifestyle. To put it plainly, this means too much sugar, too many calories, too little exercise.
So whether people develop type 2 diabetes really depends on their lifestyle. The key aspects are:
- Diet
- Exercise habits
- Body weight
Genetic predisposition also seems to play a role in type 2 diabetes. The children of someone with type 2 diabetes have a 50% chance of developing the disease themselves. To be clear, the susceptibility to possible insulin resistance is inherited, and not the diabetes directly.
Due to poor nutrition and increasing obesity among children and adolescents, these days the so-called “adult-onset diabetes” is happening at an earlier and earlier age.
In contrast to type 1 diabetes, insulin is actually still produced in type 2 diabetes.
The problem, however, is that the cell receptors no longer respond appropriately to insulin – they become blunted, or resistant. This condition is called insulin resistance. If more and more cells develop a growing resistance, type 2 diabetes develops in the long term.
Symptoms: Same as Type 1
As blood sugar rises in this way and less energy reaches the cells, the pancreas produces an increasing amount of insulin. Eventually, production is permanently exhausted here as well. As with type 1, this results in fatigue, an increased urge to urinate and extreme thirst. This is how the body tries to stabilize its fluid balance.
Type 2 diabetes develops insidiously. Since the body continues to produce insulin for a long time and the cells only gradually become resistant, the body can often compensate for this condition for years without any noticeable symptoms appearing. So in a lot of people, insulin resistance is not actually recognized until it has developed into type 2 diabetes, at which point blood sugar is already permanently raised and the majority of cells are now resistant.

Diagnosis: Only by Blood Test and Blood Sugar Measurement
Warning signs or possible indications of developing insulin resistance can show up as increased obesity and, specifically, increased abdominal fat. Along with a lack of exercise, these are the main reasons for the development of type 2 diabetes, so it’s worth having your blood sugar checked by a doctor.
In order to make a reliable diagnosis, the long-term HbA1c value is used in addition to the fasting blood sugar value. An oral glucose tolerance test can also be used to test the cells’ sensitivity to insulin. The result shows how well the cells can absorb the orally administered glucose.
In type 2 diabetes, the body still produces insulin. The problem, however, is that the cells gradually become resistant (insulin resistance) and no longer respond to the hormone. The result is an increased blood sugar level and not enough energy in the cells.
How Type 2 Diabetes Develops
Insulin resistance, which is the cause of type 2 diabetes, develops slowly. It’s a disorder in carbohydrate metabolism that results from several factors. Insulin opens the gates, so to speak, for sugar (or glucose) to enter the cell and be used as energy.
Too Much Sugar: Cell Overloade
The more sugar there is in the blood, the more insulin is secreted and the louder the signal to open the gates. If there’s now constantly too much sugar in the blood, due to a particularly high-carbohydrate diet, a lot of insulin has to be secreted permanently. This means that the cells have to work faster and faster, which overtaxes them in the long run. Their solution to protect themselves from the excessive sugar flood is to dull or reduce the number of receptors that receive the insulin signal.
Insulin Resistance Develops
In plain language, this means that the cells become increasingly resistant to insulin, which keeps the sugar in the blood. If we continue to eat too many carbohydrates and not exercise enough, this increases our insulin resistance and our blood sugar stays permanently raised. If this condition persists over a long period of time, then sooner or later it will lead to type 2 diabetes.
Causes of Type 2 Diabetes in Detail
In principle, a high-carbohydrate diet is one of the main causes of type 2 diabetes. But athletes are less affected by this. They’re able to eat a lot of carbohydrates because they also use up this energy. However, if lack of exercise and abdominal fat are added to the mix, which additionally promotes insulin resistance, then too many carbohydrates are harmful.
- High-carbohydrate diets: Large quantities of short-chain carbohydrate-rich foods in particular can prove to be too much in the long term, like sweet drinks, sweets, cakes, and pasta. They cause a large amount of glucose and insulin to flood the cell.
- High-fat diet: High-carbohydrate diets: What’s also damaging is a high-carbohydrate diet combined with fats, like, for example, sweet baked goods. Increased blood fat levels prevent the glucose from moving out of the blood and into the cells. Trans fatty acids are particularly harmful.
- Too many calories: A lot of high-carbohydrate foods are also high in calories. Too many calories can lead to an increase in abdominal fat, which in turn contributes to type 2 diabetes.
- Lack of exercise: People who don’t exercise enough don’t burn very many calories and have a higher calorie balance as a result. In addition to burning calories, exercise also promotes the absorption of sugar into the cells.
- Abdominal fat: Visceral fat, which is located in the abdomen surrounding the organs, produces pro-inflammatory substances that promote insulin resistance in cells (8).
- Obesity: About 80% of type 2 diabetics are overweight. Depending on individual body fat distribution and the degree of obesity, many overweight people also have too much abdominal fat.
- High consumption of red meat: Studies have shown that this may also contribute to type 2 diabetes (9).
- Metabolic syndrome: This is the name given to the combination of obesity, elevated blood lipids, high blood pressure, and insulin resistance, which often develops into diabetes as it progresses. The cause here, once again: the wrong diet with usually not enough exercise.
- Heredity: If there’s a family history of diabetes or insulin resistance, children have a 50% higher risk of also developing the disease. In addition to this risk, the parents’ eating and exercise habits have a significant influence on their children’s lifestyle as they get older.
- Chronic inflammatory processes: This includes silent inflammation, which can increase insulin resistance. These inflammatory processes are promoted by increased abdominal fat and its messenger substances, as well as by inflammatory triggers from diet and environment. Slightly elevated inflammatory markers can indicate inflammatory processes happening in the body.
- Magnesium deficiency: Studies show that people deficient in this vital mineral have a higher predisposition to diabetes. In contrast, high levels of magnesium can reduce the risk of developing diabetes, alleviate secondary sequelae, and improve glycemic control (10).
Before type 2 diabetes develops, insulin resistance always develops first. This happens subtly and is due to multiple factors. While a diet too rich in carbohydrates, fats, and calories, as well as a lack of exercise and obesity with increased abdominal fat usually play the biggest role, a lot of people also have a genetic predisposition to insulin resistance.
Are you interested in gaining a comprehensive understanding of the health benefits of a plant-based diet? Download the curriculum for our Holistic Nutrition Coach training program.
Consequences of Diabetes
Permanently raised blood sugar levels can result in serious illnesses. The consequences of type 1 and type 2 diabetes are mostly the same.
First, the blood vessels are damaged. Their walls are strained by the excessive sugar content of the blood and gradually lose their elasticity.
At the same time, the blood often contains clumps of platelets (thrombocytes), has an increased tendency to clot, and is more viscous in consistency. In the large blood vessels, calcification (arteriosclerosis), i.e. deposits on the vessel walls, happens over time.
These changes in the vessels can cause the following health problems:
- Circulatory disorders (in toes and feet, these can lead to what’s called diabetic foot, which can result in amputations).
- Poorly healing wounds
- Eye problems
- Dementia
- Heart attack
- Stroke
- Kidney failure
- Nerve damage (diabetic polyneuropathy)
Is Type 2 Diabetes Curable?
As long as the pancreas is still able to produce insulin – and this is usually the case with type 2 diabetes – we now know that type 2 diabetes is curable. For a long time, this was not a recognized fact. Diabetes, both type 1 and 2, was considered a chronic metabolic disease that, once diagnosed, would not go away.
But today, there are plenty of examples of type 2 diabetes being cured: Cells can become more sensitive to insulin again, even to the point that diabetes will actually go into “remission;” or in other words, it regresses. There are even cases of healing with type 1 diabetes – as well as in other autoimmune diseases. But there’s a much lower chance of this happening than in type 2 diabetes. The necessary steps to be taken, however, are the same.
To achieve a cure or even an improvement, making fundamental changes in lifestyle is crucial – especially eating and exercise habits. For most people, an important aspect is reducing body weight, especially abdominal fat.
As long as the body is still producing its own insulin, type 2 diabetes can go into remission. That is, the body can heal and carbohydrate metabolism can normalize.
Holistic Measures for Diabetes
The same recommendations apply to both type 1 and type 2 diabetes. To summarize, the goal is to replace the habits that led to the disease in the first place with new sensible and healthy habits – permanently.
Reduce Carbohydrate Intake
Diabetes is a carbohydrate metabolism disorder caused mainly by too many carbohydrates. To relieve the body and make the cells more sensitive again, it’s crucial to reduce carbohydrates in the diet. Sugar is the simplest form of carbohydrates, and industrially processed sugar in particular often contributes considerably to insulin resistance.
Foods or products that contain carbohydrates in large amounts and in isolation, which means without the simultaneous presence of protein and fiber, should also be avoided. These include sweet drinks, sweets, cakes, desserts, pasta, and fruit juices. When it comes to juice, it’s much better to use fresh vegetable juice instead of fruit juice.
Low-Fat Diet
An additional burden on the insulin balance is a high-carbohydrate diet combined with a high-fat diet. If there are too many fat droplets in the blood, a thin film of fat can form on the walls of the blood vessels, the place where the insulin receptors of the cells are located. This prevents the glucose from being removed from the blood and into the cells. Trans fatty acids are particularly harmful.
Adjust Energy Intake and Lose Weight
Most people with diabetes are overweight. The main reason for this is a positive energy balance, which means that more calories are consumed than the body needs. To lose weight and also belly fat, a negative balance is needed. This can be reached by eating lots of vegetables and foods that are filling and protein-rich, like nuts and seeds. Highly industrially processed products, which often have a lot of calories, should be eaten less or just avoided altogether.
Natural Foods
The key to health is natural foods. These provide the body with all the nutrients it needs, and the result is a natural and healthy satiety. Fresh vegetables, wild herbs, low-sugar fruits, nuts, oilseeds, and sprouts should form the basis here. Carbohydrate side dishes like millet, buckwheat, brown rice, and quinoa can be integrated in small amounts and in combination with other foods.
Eating: Regularly and Mindfully
The body can adjust really well to regular meals at appropriate intervals of about four to five hours. While constant snacking promotes obesity and insulin resistance, meal breaks that are too long can put the body in a state of emergency, where it bunkers its energy. It’s equally important to eat and enjoy food calmly, consciously, and mindfully, by using all the senses. Thorough chewing plays a major role here. This is the best way for the pancreas to deal with carbohydrates.
Sufficient Exercise
Along with the right diet, exercise is the cure for diabetes and insulin resistance. It’s been proven that exercise improves the insulin sensitivity of the cells. But we’re not just talking about strenuous exercise: any exercise counts, whether it’s climbing stairs, going for a walk, or hanging out the laundry. Exercise in the fresh air is especially valuable, since this helps form additional vitamin D through exposure to sunlight.
Avoid Meat and Sausages
High ferritin (“storage iron”) levels are often found in people with diabetes. This may show that too much iron actually contributes to diabetes, because excessively high ferritin levels can lead to oxidative stress and damage to pancreatic cells. Since meat and sausage products contain a lot of iron, they should also be avoided.
Omega-3 Fatty Acids
Good fatty acids have an anti-inflammatory effect and help reduce any inflammation in the body, which supports insulin resistance. Those who regularly use omega-3 fatty acids from chia seeds, hemp seeds, linseed, or linseed oil can reduce their risk of developing diabetes.
High-Quality Water
Without a sufficient amount of water, which would be about 1.5 to 2 liters daily, our metabolism cannot function in its ideal capacity. Especially in the case of insulin resistance or diabetes, where the body produces more urine and excretes more fluid, water intake is incredibly important.
Supplement Micronutrients
Certain micronutrients are especially important for a well-functioning sugar metabolism:
- Magnesium: Is found in pumpkin seeds, sunflower seeds, quinoa, and almonds. Additional magnesium can also be taken through dietary supplements or magnesium-rich foot baths.
- Chromium: The trace element plays a crucial role in sugar metabolism: It improves insulin sensitivity and regulates insulin secretion. Good sources of chromium are seeds and sprouts, especially lentil sprouts.
- Zinc: This mineral has all kinds of important functions in the body – among other things, zinc has an antioxidant effect, which supports cell health, and also has an anti-inflammatory effect.
Instead of having to take medication or inject insulin for the rest of your life, it’s possible to improve insulin sensitivity and possibly cure diabetes altogether with a holistic lifestyle that includes, above all, a healthy diet and plenty of exercise.
Valuable articles on the subject:
You are interested in gaining a comprehensive understanding of the health benefits of a plant-based diet?
Take the opportunity and join our unique, based on nutritional sciences and practice-oriented training program for gaining a high level of health.
We are more than happy to inform you about our training program on our website!




0 Comments